Can AI Help To Treat The Mental Health Crisis?
July 20, 2018

By Ciarán Daly
LONDON, UK - Today, mental health conditions are endemic. There is widespread consensus that society is facing an unprecedented rise in mental health conditions. Mental health is frequently described as being in ‘crisis’; something that fiscally strained health services simply do not have the resources to either treat or prevent.
You don’t have to look far to find statistical evidence in support of this. Today, over 40 per centof all GP appointments in the UK concern patients’ mental health, while the British NHS has seen a sharp rise in patients under the age of 19seeking treatment from mental health services. In 1980, 4% of Americans suffered a mental disorder associated with anxiety—these days nearly halfof the population does.
The jury is still out as to whether we are witnessing an actual rise in the number of mental health conditions, or if better public knowledge and education has led to a growth in people seeking diagnosis and treatment. What is clear, however, is that there remain a number of significant obstacles to improving the mental health of populations worldwide, with major implications for not only society but the economy as well. From 2013 to 2016, for example, an estimated 45 million working daysin the UK were lost due to stress, anxiety, and depression.
Towards a data-driven treatment programme
One of the major obstacles lies in the design and delivery of effective, appropriate treatments. Nowhere is this truer than depression. While published trials demonstrate that antidepressants and psychotherapy can reduce symptoms by 45 to 60%, for example, there’s no way to know how effective a certain treatment will be for an individual patient. The prospect of AI and genomics-powered ‘personalized’ medicine has been grabbing the headlines for some time now, but developers remain some way off from a marketable product.
What can be personalized and augmented today, however, is the choice of treatment path itself. There’s no shortage of data when it comes to measuring depression, or indeed patient health records—providing some hope of building an intelligent analytics solution. Psychiatrists and physicians have employed a range of measures to assess patient symptoms for nearly 60 years. Many of these measures take the form of questionnaires or self-reporting: a 9-point questionnaire is used to screen patients for depression, while factors such as sleep, physical activity, hours spent socialising, and quality of life are continually measured thereafter.
“Clearly the problem most in need of a new technological solution is not diagnosis. It’s very difficult to choose a treatment for patients with depression—there’s an awful lot of them, and there’s no way to know who will actually respond to drug A or therapy B in an accurate fashion,” explains David Benrimoh, CEO of Aifred Health.
Founded to compete in the IBM Watson AI xPrize, Aifred Health are pioneering a tool that clinicians are able to use in partnership with patients with depression to make better, data-informed decisions about their treatment. The hope behind Aifred is to reduce the amount of time to takes people to recover, the risk of relapse and suicide, and, ultimately, patient suffering.
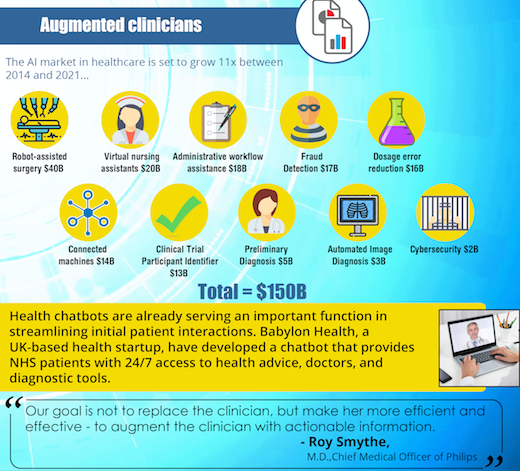
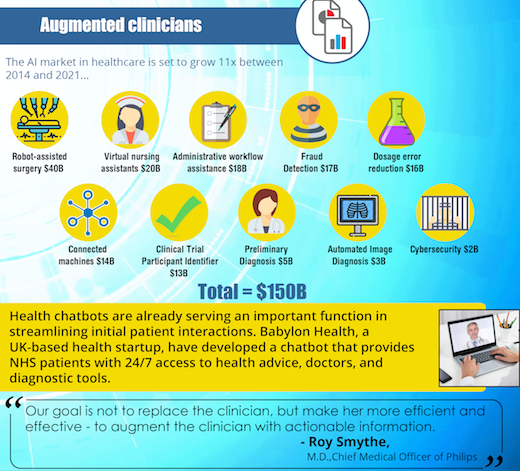 Related: 5 Ways AI Will Transform Healthcare [Free Infographic]
Related: 5 Ways AI Will Transform Healthcare [Free Infographic]
Build AI models using domain expertise
The obstacles to building an AI tool for depression then lies not so much in how a condition is measured, though this could certainly be improved based upon patient update, says Benrimoh, but in assessing the relationships between the variables making up that condition. This is something only be achieved through close collaboration with clinicians.
“You need to build AI models using domain expertise. It’s not the kind of thing you can just throw engineers at by themselves and expect something useful to come out of it,” Benrimoh argues. “Having the experience to know what makes sense at a clinical level is incredibly important.”
By combining teams of clinical experts, neuroscientists, data scientists, and software engineers, it’s possible to develop a deep learning model that continuously assesses all the complex relationships between variables making up a condition and predicts probabilities of response to different treatments. This is where patient data becomes truly valuable—as well as a risk factor.
For a solution like Aifred to work, it has to track patient symptoms continuously in order to assess results and improve the deep learning model in place. While this can drive superb outcomes, anything that involves individualised tracking of highly sensitive data is bound to raise a few eyebrows.
Technology can only improve outcomes alongside a bold social approach
A black box algorithm that makes opaque decisions can pose some problems for, say, a financial services firm, but when it comes to mental health, there are lives on the line. Benrimoh insists, however, that Aifred thankfully not only has explainability built into its core, but that explainability is vital for clinicians to be able to make effective prognoses.
“While the complaints about deep learning being a ‘black box’ are valid when you’re looking at, say, image analysis, the beauty of what we’re doing here is that all the data is based on questions and pieces of clinical information,” says Benrimoh. Using questionnaire data enables the software to extract vital information and, crucially, compile clinical reports that explains why the system has predicted a certain response to a specific treatment.
Applications like Aifred will no doubt grow and expand their functionality; Benrimoh says the firm will begin to potentially look at applying the software to schizophrenia, anxiety, bipolar disorder, and addiction further down the line. However, in a society where loneliness and mental health reach epidemic proportions, nobody would suggest that technology holds all the answers. AI is one component of a much-needed holistic approach to overhauling our approach to health care and prevention.
“Let’s say we’re able to treat people faster. Okay, great. Do we then have the services in place to help people get back to work faster? If our support system predicts that psychotherapy is a great treatment for most patients, do we then have the systemic capacity to ensure there’s enough psychotherapists to deliver that treatment?” Benrimoh asks. “These are the kinds of socio-political and economic questions that need to be asked when you’re building something like this. If you really want to change a social problem, it’s a question of social programmes, and within those, AI can help us.”

Based in London, Ciarán Daly is the Editor-in-Chief of AIBusiness.com, covering the critical issues, debates, and real-world use cases surrounding artificial intelligence - for executives, technologists, and enthusiasts alike. Reach him via email here.
About the Author(s)
You May Also Like


.jpg?width=700&auto=webp&quality=80&disable=upscale)
.jpg?width=700&auto=webp&quality=80&disable=upscale)
.jpg?width=700&auto=webp&quality=80&disable=upscale)
.jpg?width=300&auto=webp&quality=80&disable=upscale)
.jpg?width=300&auto=webp&quality=80&disable=upscale)

.jpg?width=300&auto=webp&quality=80&disable=upscale)
.jpg?width=300&auto=webp&quality=80&disable=upscale)